AI is changing how the healthcare industry handles data from early diagnosis to real-time risk monitoring and clinical decision support. Turning sensitive, fragmented clinical data into actionable insights requires more than just AI models. It also demands compliance, the right tech stack, and use-case precision.
We'll break down how AI-driven data analysis is reshaping healthcare, with a focus on high-impact outcomes, regulatory readiness, and deployment best practices.
Unique Challenges in Healthcare Data Analysis
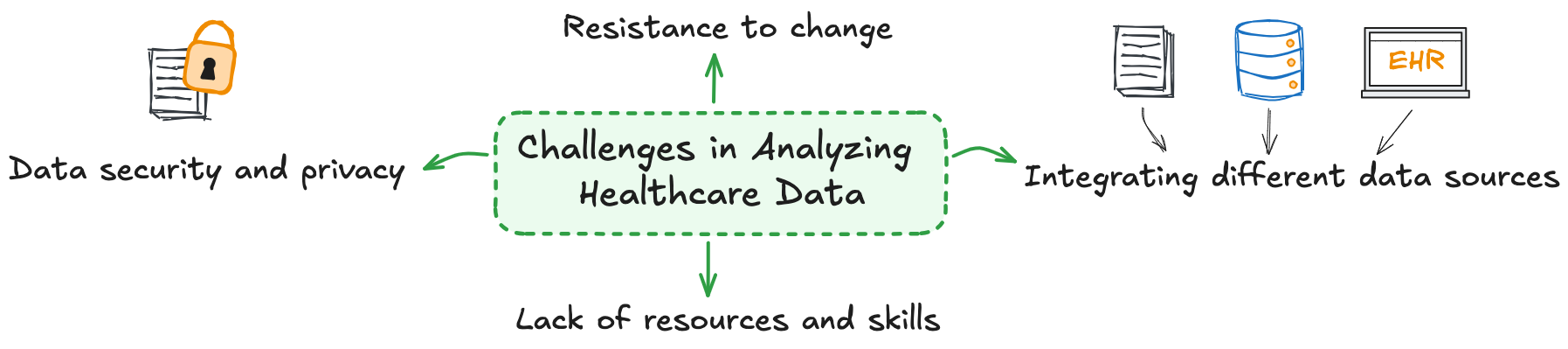
Healthcare data comes from many disconnected sources: patient records, lab results, medical scans, insurance claims and doctor’s notes. A single patient’s history might be split across multiple hospitals, buried in legacy systems, or somewhere in PDFs and handwritten forms that defy easy extraction.
Electronic Health Records (EHRs) were meant to fix this. By digitizing the core components of patient care (like diagnoses, medications, allergies, lab values, and clinical notes), EHRs replaced paper charts and made it easier to store and retrieve information. But adoption has been uneven, and resistance to change remains common, especially among smaller providers with limited budgets or IT staff.
Even where EHRs are in place, they rarely tell the full story. Many exclude essential clinical data such as medical images, pathology slides, genomic sequences, and behavioral health notes. Crucially, most EHR systems don’t communicate with each other. Each provider may run on a different platform, and data interoperability is still more aspiration than reality. This leads to fragmented, duplicative, and incompatible records that are difficult to reconcile, let alone analyze. Explore more about the challenges of Data Integration.
From the analyst’s point of view, this complexity becomes a bottleneck. Data is often messy — inconsistent across sources, poorly structured, and scattered across formats. Natural language dominates clinical notes, and critical insights may be locked in scanned documents or messy databases. On top of this, many healthcare teams lack the internal data science capacity or tooling to clean and organize this information at scale.
And then there’s compliance. Privacy laws like HIPAA and GDPR place necessary constraints on how data can be accessed, used, or shared. These safeguards are vital for protecting patient rights, but they also introduce technical and legal hurdles for anyone trying to train models, run cohort analyses, or generate real-time alerts. In healthcare, you don’t just need data — you need it fast, secure, and interpretable, or someone might pay the price with their life.
Regulatory Landscape (HIPAA, GDPR-Health)
Privacy laws define the boundaries of what’s possible with patient data, and crossing those lines isn’t optional. In the U.S., the Health Insurance Portability and Accountability Act (HIPAA) sets the rules for how patient information can be collected, stored, and shared. It requires encryption, access controls, and detailed audit logs to protect sensitive health data.
In the EU, the General Data Protection Regulation (GDPR) goes even further. It gives patients full control over their data, requires explicit consent for its use, and demands transparency around how AI models process health records.
If you’re using AI to analyze lab results, patient notes, or medical images, the tool must be fully HIPAA or GDPR compliant. That means secure storage, anonymization when needed, role-based access, and clear reporting features. If these aren’t built in, the tool isn’t legally usable at all.
High-Impact Use Cases
Despite the challenges, AI is already improving healthcare by boosting efficiency and delivering better outcomes. These are some of the highest-impact use cases today:
Patient Risk Stratification
AI models can analyze EHRs, lab results, and clinical notes to identify patients at high risk of readmission, deterioration, or complications. Hospitals use this to prioritize interventions, reduce length of stay, and improve population health metrics.
Imaging & Diagnostics
Computer vision models combined with structured data can improve accuracy in radiology, pathology, and dermatology. Analysts use AI to surface patterns in scans that physicians might miss, speeding up diagnosis and reducing false positives.
Clinical Trial Optimisation
AI helps accelerate patient recruitment by matching candidates based on eligibility criteria mined from real-world data. It can also predict dropout risks, monitor adherence, and uncover adverse event patterns faster than manual review.
Technology Stack & Vendor Shortlist
The right tools are those that balance performance, compliance, and usability. Look for:
-
HIPAA-compliant platforms that offer encryption, audit trails, and role-based access
-
Real-time data capabilities for monitoring, alerts, and time-sensitive analytics
-
Natural language interfaces for clinical users who need fast insights without writing code
A few vendors to consider are: Briefer (agent-native analytics, HIPAA-ready), Microsoft Fabric (tight Excel and Power BI integration), Databricks Mosaic (scalable AI pipelines for health data), and open-source tools like PandasAI or DuckDB for in-house development.
For a broader look at AI across industries and use cases, check out our Best AI Tools for Data Analysis guide.
Implementation Framework (Data Governance to Deployment)
To apply AI in healthcare the right way, start by making sure the basics are clear: who can access patient data, how consent is handled, and how clinical staff will review the system’s outputs. Then, test everything in a safe environment, using fake or anonymized patient data so there’s no risk to real people while you're still experimenting. You can check our full guide on Exploratory Data Analysis with AI to learn more about this process.
Once tested, set up a system that can go from looking at past data to analyzing live information as it comes in. Keep an eye on your AI as it runs: over time, it might get less accurate as real-world conditions change or new types of patients appear. If you're not monitoring it, you won’t know when it starts making bad calls.
When it's time to launch, don’t drop it all at once. Roll it out in stages, with doctors, analysts, and engineers all involved. The goal is to improve it continuously, based on feedback.
Data Security & Ethical AI Checklists
Make sure your AI workflows include:
-
End-to-end encryption (at rest and in transit)
-
Fine-grained access controls
-
Model explainability and human review loops
-
Transparent data use policies for patients
-
Ongoing audits and fairness assessments
-
Ethical AI use.
Future Outlook: Genomics, Wearables, Multi-Modal AI
The next wave of healthcare AI will go beyond structured records. Expect deeper integration with genomic data, wearable health trackers, and multi-modal analysis that blends text, images, and real-time vitals. LLMs and agent-based platforms will increasingly act as decision support partners for both analysts and clinicians.
Additional Resources
Ready to go deeper? Our AI learning path includes real-world tutorials, tool walkthroughs, and example workflows tailored to healthcare analytics teams.
